Learning Center: Access information in greater detail.
Gastric feeding tube (G tube) placement considerations
Whether and when to undergo placement of a G tube (or nasogastric tube) when undergoing treatment for head and neck cancer is a commonly encountered decision.
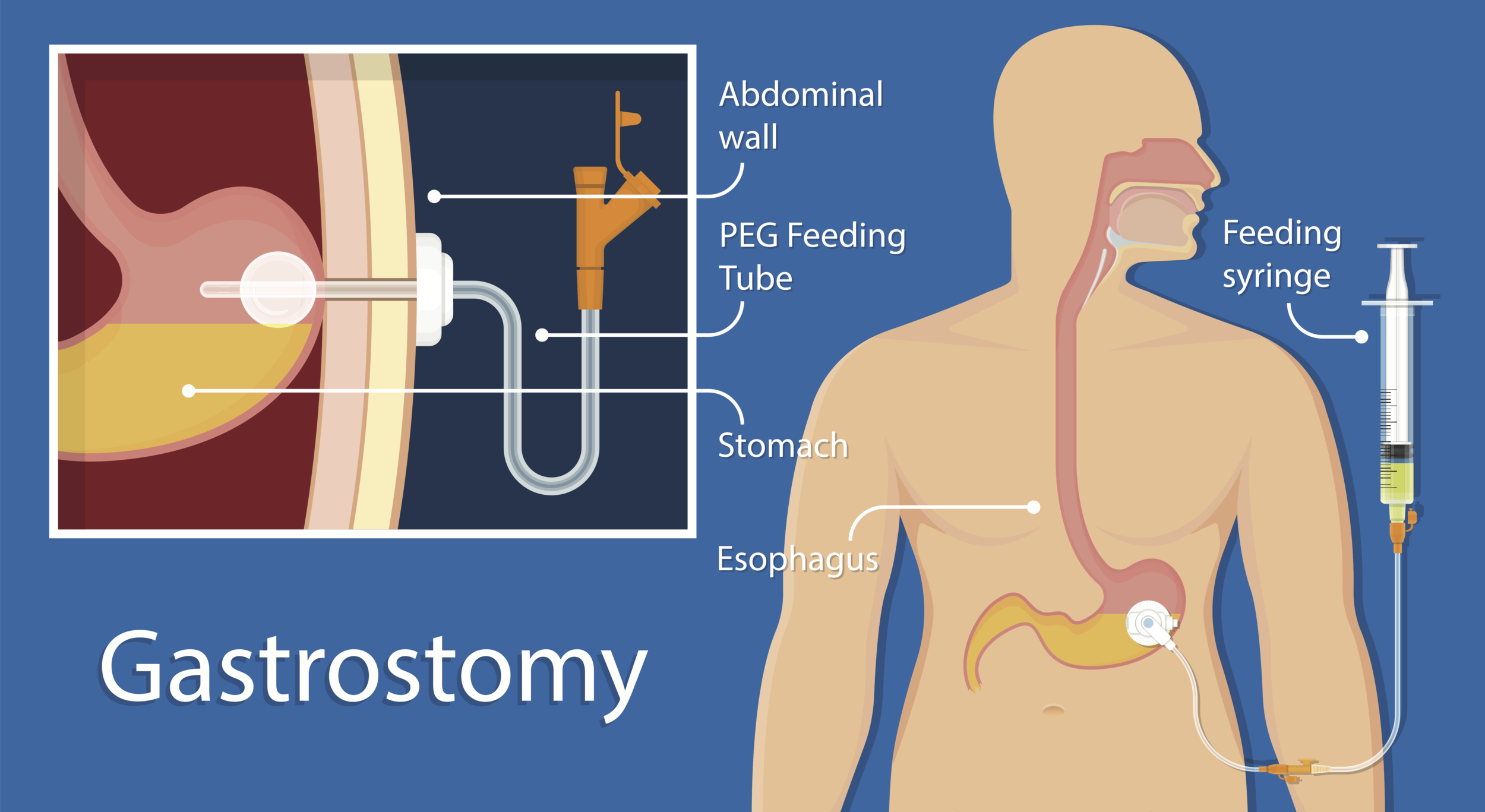
A gastrostomy feeding tube (G-tube) is a tube that passes through the skin of the abdomen directly to the stomach.
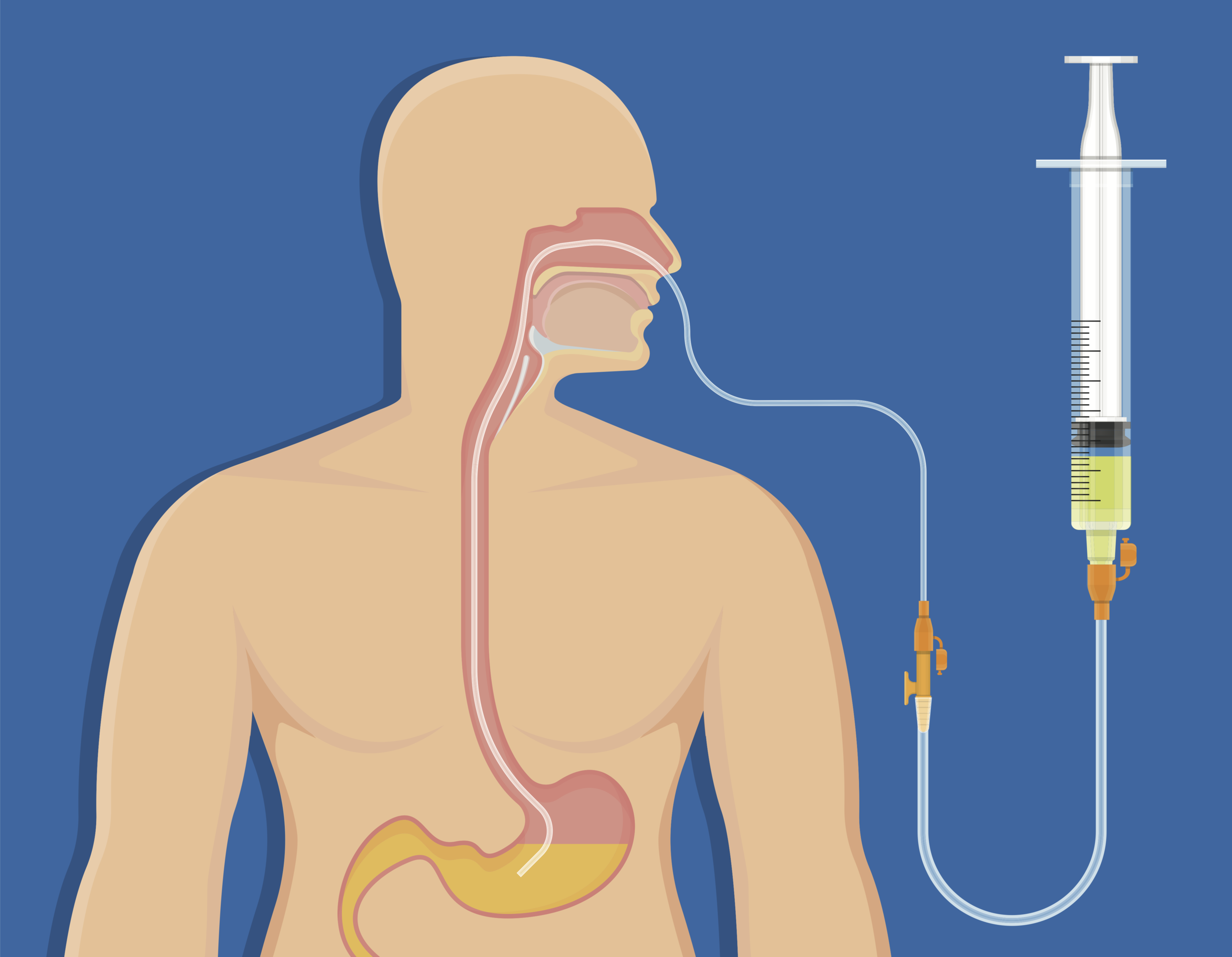
A nasogastric feeding tube (NG tube) is a tube that passes through the nose, down the throat and esophagus to the stomach.
background: why a gastric feeding tubewould be considered
Swallowing efficiently, and safely without significant discomfort is necessary for nutrition and general health. Treatment of a tumor of the mouth, throat, or larynx can make swallowing problematic. This especially concerning for patients in whom the cancer itself has already led to poor nutrition or lung infection due to aspiration (food or liquid going down the windpipe). Typically, for head and neck cancer, the digestive tract from the esophagus down is fully functional, so a way to route food and liquid into the stomach via a tube passing from the abdominal wall is an effective solution. Another way to get food, liquid, and medicine into the stomach without requiring swallowing is via a nasogastric tube, which is passed from one nostril, down the throat and esophagus, into the stomach.
ADVANTAGES OF A G TUBE (through the abdominal wall)
Having a G tube provides an easy way to get nutrition, hydration, and medications into the stomach. A G tube hides well under a shirt and usually other people are unaware of its presence. A G tube may be removed when no longer needed and the abdominal wound typically heals closed quickly without additional surgery. Having a G tube does not prevent someone from eating and drinking by mouth; the G tube can be a backup in case additional food or hydration is needed beyond what someone takes by mouth.
DISADVANTAGES OF A G TUBE (through the abdominal wall)
G tube placement is a procedure with some risk. The abdominal wound from a G tube sometimes requires additional medical attention and gastric juices can sometimes leak around the tube to the outside of the body, causing skin irritation. Most people have a sore abdomen (the sit-up muscles, in particular) after G tube placement for about 3 days. Perhaps most importantly, however, is that since maintaining motion and mobility of the throat and oral cavity requires active use of the throat and oral cavity, having an easy out to bypass chewing and swallowing motion can lead to long-term swallowing disfunction, and even need for long-term G tube usage. In other words, radiation and chemotherapy plus radiation cause a sore throat and swallowing can be painful. However, scar tissue begins to set in during treatment and new scar tissue continues to be formed after radiation. This scar tissue is stiff and stiffness is very disruptive to normal swallowing function. Unless the swallowing muscles are being used frequently every day, scar tissue stiffness can make swallowing very slow and arduous or even unsafe. Swallowing regularly during and after therapy is essential whether one has a G tube or not if long-term swallow function is to be preserved.
Advantages of a nasogastric feeding tube
The main advantage of a tube passing from a nostril to the stomach is that it does not require any incision and can be performed quickly without as much preparation and planning as the gastrostomy tube. It may be removed easily as well.
Disadvantages of a nasogastric feeding tube
The main disadvantage of a tube passing from the nostril to the stomach is discomfort. It is typically considered moderately uncomfortable for the first fifteen or so minutes, before a person habituates to its presence, but then it remains somewhat uncomfortable usually for as long as it is in place. Another significant disadvantage of this type of tube is that one cannot be discharged from the hospital with one in place owing to the chance it might slip out just enough for the tip to position above the larynx, making aspiration of tube feedings into the lungs a risk. Having the tube slip out completely is another risk for home use because a patient may not be able to eat, drink, or take medicines until the tube were replaced, which usually requires a return trip to the hospital.
my usual recommendations
Each situation is individual and my advice is tailored to a patient’s situation. Young, motivated, otherwise healthy and robust patients in general have a better chance of gleaning the benefit of maintaining swallowing function without compromising nutrition or risking lung infection without a feeding tube, whereas the already malnourished patient who has bad lungs or swallowing already compromised by the tumor may be best served by having a G tube placed early in the process, such as before treatments being. I typically use nasogastric feeding tubes if the expected duration of use is less than about five days. Talk with your doctor about specific recommendations.
Removal of a Feeding tube
Generally, removal of a G tube may be undertaken when it is highly likely the patient no longer needs it. In my practice, when it appears as if the gastric feeding tube may no longer be necessary, I usually like to see a patient maintain or gain weight with an oral diet (not using the G tube at all) for one month, before I think it is safe for G tube removal. The risk of removing the G tube before someone can sustain adequate intake by mouth is that weight loss and dehydration may occur, and the G tube may need to be replaced in a repeat procedure. Removal of a G tube is typically undertaken by the physician who placed it originally, or one of their partners, who will also provide wound care instructions.
Removal of a nasogastric tube is simpler undertaking. Any retaining stitch or tape holding the tube in place is removed and the tube may be pulled out. Because of the simplicity of removing a nasogastric tube as well as the relative simplicity of replacing it, if necessary, criteria to meet before removing a nasogastric tube are usually less stringent than with a G tube.
Learning Center Main Index:
Throat:
swallowing, tonsils and adenoids, obstructive sleep apnea, voice
Aesthetics:
skin regimen, injectables {neuromodulators (e,g. Botox), hyaluronic acid fillers (e.g., Juvederm), and others}, rhinoplasty, facelift, neck lift, and brow lift, blepharoplasty (eyelid surgery), skin resurfacing, scar treatment
Tumors (benign and malignant/cancerous):
general tumor information, thyroid, parathyroid, skin, neck, oropharynx, larynx (voice box), salivary gland, nose and sinus, oral cavity (mouth and lips), nasopharynx, hypopharynx, radiation therapy, chemotherapy and immunotherapy, gastric feeding tube
Nose and Sinus:
rhinoplasty (functional and cosmetic), sinusitis, breathing