Learning Center: TONSILS AND ADENOIDS
Access information in greater detail.
Use the search tool or scroll down for your topic of interest.
ANATOMY OF THE TONSILS AND ADENOIDS
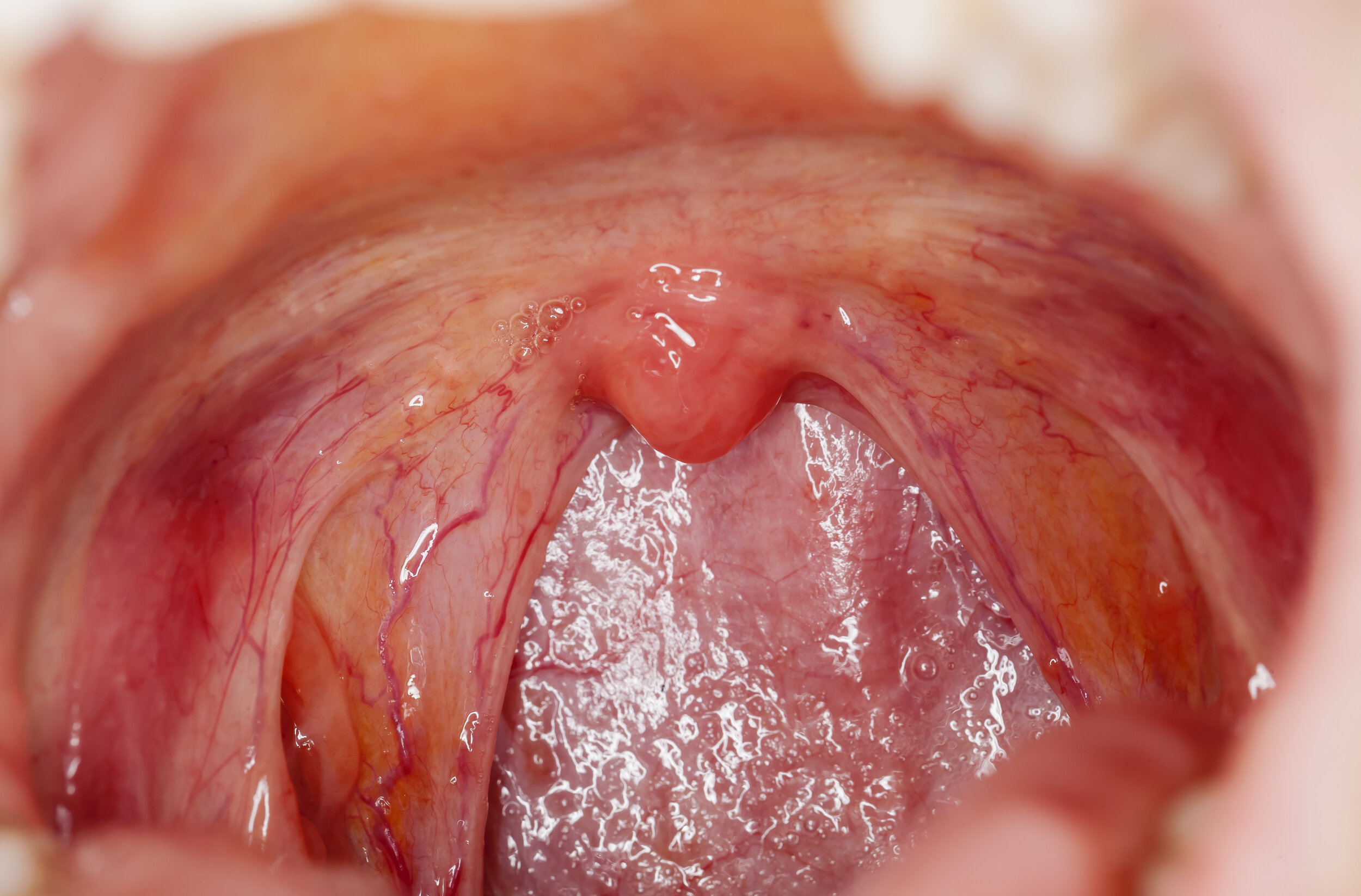
Large tonsils seen behind the tongue on the left and right.
Minimal to no tonsil tissue present.
Adenoids are located at the “corner” between the back of the nose and the top of the throat.
FUNCTION OF THE TONSILS, ADENOIDS, and lingual tonsils
The tonsils, adenoids, and lingual tonsils are composed of lymphoepithelial tissue, which is rich in immune system cells, whose immune system purpose is complete early in life. To date, there are no studies that demonstrate a significant clinical impact of tonsillectomy or adenoidectomy on the immune system, but tonsils, adenoids, and the lingual tonsils, often cause health problems, with infections, airway blockage, or tumors.
Tonsillectomy for recurrent throat infections in children
Given the high numbers of throat infections and the number of tonsillectomies performed, a great deal of research has been devoted to indications for tonsillectomy in children, taking into account risks, benefits, and alternatives. Current guidelines are that the number of recurrent throat infections should be at least seven infections in the past year, at least five per year for two years, or at least three infections per year for the past three years. Documentation for an episode should include a sore throat at at least one of the following: temperature of at least 38.3°C (101°F), enlarged neck lymph node(s), discharge (exudate) on the tonsils, or a positive test for “strep” (group A beta-hemolytic streptococcus). Alternative indications for tonsillectomy, regardless of the numbers of throat infections include situations in which the child has had multiple peritonsillar abscesses, multiple antibiotic intolerances or allergies, or “Periodic Fever, Aphthous Stomatitis, Pharyngitis, Adenitis” (PFAPA), which is a syndrome of repeated episodes of fever, mouth sores, sore throat, and swollen lymph nodes.
Tonsillectomy for Obstructive Sleep Disordered Breathing in Children
As with the above, good research has led to development of guidelines for tonsillectomy for obstructive sleep disordered breathing, which state that for children age two or older with large tonsils as well as some evidence of poor sleep (poor school performance, behavioral problems, growth retardation, or bed-wetting), tonsillectomy is a good option. If the child is less than two years old or has a medical condition of Down syndrome, obesity, craniofacial abnormality, neuromuscular disease, sickle cell disease, or mucopolysaccharidosis, an overnight sleep study (polysomnogram) is indicated, before tonsillectomy is undertaken; if obstructive sleep apnea is diagnosed, tonsillectomy is recommended. Tonsillectomy helps almost all normal-weight children with obstructive sleep disordered breathing. Tonsillectomy also helps overweight children with obstructive sleep disordered breathing but sleep is not always improved.
Other reasons for tonsillectomy
Chronic (long-lasting) tonsillitis, difficulty swallowing due to tonsils, and suspicion for tonsil cancer are reasons for tonsillectomy. Recurrent sore throats in adults do not have evidence-based guidelines as noted above for children, but the idea is the same. Halitosis (bad breath) and tonsilloliths (tonsil stones) are possible reasons for tonsillectomy. Risks, benefits, alternatives and the expected outcomes should be discussed with your doctor prior to undertaking any procedure. Tonsillectomy is generally recommended after a second peritonsillar abscess.
WHEN AND WHY TO REMOVE ADENOIDS?
Adenoids are typically removed when:
The tonsils are being removed and the adenoid pad, inspected during the surgical procedure, is found to be enlarged.
A second set of pneumatic equalization ear tubes is being placed.
Adenoid enlargement is identified as a cause for nasal obstruction.
Adenoid infection is identified as a cause for chronic symptoms such as nasal discharge.
Considerations for tonsillectomy in children for obstructive sleep disordered breathing
Enlarged tonsils is the most common reason that children develop obstructive sleep disordered breathing.
Obstructive sleep disordered breathing is not solely due to enlarged tonsils; muscle tone also plays a role.
Obesity plays a major role in obstructive sleep disordered breathing.
A polysomnogram (sleep study done in the sleep lab) is considered the best test to confirm that the child has obstructive sleep apnea which would benefit from surgery.
A polysomnogram is not necessary in all cases and access may be limited by availability of sleep laboratories and willingness of insurers and third-party payers to cover the cost of testing. For an otherwise healthy child with a strong history of struggling to breathe with daytime symptoms of enlarged tonsils, a polysomnogram is typically not performed unless the parents want to confirm the diagnosis.
The success of tonsillectomy is variable. The age, weight, ethnicity, severity of obstructive sleep disordered breathing, and associate medical conditions all affect the success. Younger, normal weight, non-African-American children may have a resolution of obstructive sleep disordered breathing of 80%.
For obese children, tonsillectomy produces complete resolution of obstructive sleep disordered breathing < 50% of the time.
Caregivers need to be aware that their child may require additional interventions to cure his/her obstructive sleep disordered breathing which can vary from weight loss, medications, or wearing a special mask while sleeping that will keep the airway open. Some children may be candidates for more advanced sleep surgery procedures.
Additional links
Learning Center Main Index:
Throat:
swallowing, tonsils and adenoids, obstructive sleep apnea, voice
Aesthetics:
skin regimen, injectables {neuromodulators (e,g. Botox), hyaluronic acid fillers (e.g., Juvederm), and others},rhinoplasty, facelift, neck lift, and brow lift, blepharoplasty (eyelid surgery), skin resurfacing, scar treatment
Tumors (benign and malignant/cancerous):
general tumor information, thyroid, parathyroid, skin, neck, oropharynx, larynx (voice box), salivary gland, nose and sinus, oral cavity (mouth and lips), nasopharynx, hypopharynx, radiation therapy, chemotherapy and immunotherapy, gastric feeding tube
Nose and Sinus:
rhinoplasty (functional and cosmetic), sinusitis, breathing